What Is Urinary Incontinence?
Urinary incontinence, also known as UI, is a common condition that involves the involuntary loss of urine. Although it is not usually a serious condition, UI can be embarrassing and affect a person’s daily life. Urinary incontinence is most common in women, especially during and after pregnancy, but can affect people of all ages.

Is an “overactive bladder” the same as urinary incontinence?
Overactive bladder is a condition in which the bladder can no longer hold urine normally. If you have an overactive bladder, you might often feel a sudden urge to urinate or experience an accident.
Urinary incontinence could be the result of an overactive bladder if you experience involuntary loss of urine. However, they’re not the same thing. Incontinence can be a result of an overactive bladder.
The Causes Of Urinary Incontinence
Urinary incontinence is often caused by a urinary tract infection or weak muscles in the urinary tract. Some medications may cause weak bladder muscles, therefore causing urinary incontinence. Weak muscles may prevent the closing off of the urethra, and doing certain activities may cause urine to leak. Normal urination involves emptying the bladder when the desire to urinate occurs, at which point the bladder contracts and flows out of the body. Once the bladder is empty, the muscles contract and urination stop. People with UI experience a disruption in this process that causes a loss of bladder control and results in troubling symptoms.
What Our Patients Have To Say
“What can I say, Dr. ROBERTS is amazing! She is one of the best Gynecologist I’ve ever had the pleasure of meeting. Her staff is just as amazing as she is, love their office!!”
– Mara G.
"I’ve been seeing Dr. Joyner for many years. She is truly genuine yet extremely professional and informative. I cannot recommend her enough. She makes what could be an awkward experience one that is easy. We moved 100 miles away but I will continue to use her because it’s simply worth it."
– Lexie Manson
What Are The Symptoms Of Urinary Incontinence?
In addition to leaking urine, people with UI may also experience:
- Strong desire to urinate
- Pelvic pressure
- Frequent urination
- Nocturia, or the need to urinate at night while sleeping
- Painful urination
- Bed wetting

UI is a common condition with many treatment options that can relieve symptoms and allow patients to perform their regular activities without the embarrassment and worry of urinary leakage.
The 3 Types Of Urinary Incontinence
Urinary incontinence may be classified into three different types based on causes and symptoms.
Urge Incontinence
Urge incontinence is the most common type of incontinence. This type of incontinence involves urine leakage that occurs after a sudden urge to urinate because the muscle wall of the bladder is overactive.
Stress Incontinence
Stress incontinence is defined as urine leakage that occurs after an activity places pressure on the bladder. Activities may include coughing, laughing, or sneezing.
Overflow Incontinence
Overflow incontinence occurs as the result of an inactive bladder muscle that does not completely empty the bladder after urination. This is the least common of the types of incontinence.
Does pregnancy cause a lasting problem with incontinence?
Roughly 40 percent of women have some degree of urinary incontinence during pregnancy. This is caused by the growing fetus pushing down on the woman’s bladder, urethra, and pelvic floor muscles. Over time, this pressure may weaken the pelvic floor muscles and lead to leaks or problems passing urine.
Most of these problems with incontinence during pregnancy go away after childbirth when the muscles have had some time to heal.
How does urinary incontinence relate to age?
Urinary incontinence is more prevalent as people get older, as support tissues and muscles weaken or loosen. It isn’t an absolute — lifestyle changes and treatment can ease the problem — but there is definitely a relationship. The aging of the bladder muscle can decrease the bladder’s capacity to store urine. Plus, involuntary bladder contractions become more frequent with increasing age.
There is a relationship with menopause. After a woman exits menopause, she is producing less estrogen, and this is necessary to keep the lining of the bladder and urethra healthy. Deterioration of these tissues can lead to incontinence.
How Urinary Incontinence Is Diagnosed
Patients exhibiting the symptoms of UI should see their doctor determine the cause, type, and severity of their condition. Doctors can diagnose urinary incontinence through a series of tests and an evaluation of the patient’s medical history. Patients may also be asked to keep a bladder or urination diary to record the frequency and circumstances of their urination troubles. Testing may begin with a pelvic exam to detect any physical abnormalities, and may also include:
- Blood tests
- Urinalysis
- Cystogram
- A stress test to determine if any urine leaks during physically stressful situations
After a diagnosis of UI, the physician may perform further testing to determine the cause of the condition, in order to recommend the most appropriate treatment approach.
Urinary Incontinence Treatment
There are many different treatment options available for urinary incontinence, depending on the severity of the condition. Conservative treatments are often effective, and may include:
- Bladder training
- Avoiding alcohol and caffeine
- Medication to control pelvic muscle spasms.
- Kegel exercises

For more severe cases, a medical device such as a urethral insert or pessary may be inserted through the vagina to prevent urine leakage. Surgery may also be recommended to provide support to the bladder neck to relieve symptoms caused by UI. However, there are certain risks associated with surgery, including infection, bladder spasms or recurring incontinence. A doctor will determine which treatment is best for each patient after a thorough evaluation of their condition.
What are Kegel exercises and how do they help with incontinence?
Kegel exercises, also known as pelvic floor training, are exercises used to strengthen the pelvic floor muscles to help prevent or reduce urinary incontinence. These muscles support the uterus, bladder, small intestine, and rectum.
Four in 10 women see improvement in managing their incontinence after adopting a regimen of Kegel exercises. They can be especially helpful during pregnancy to overcome some of the weakening of the pelvic floor muscles. Kegel exercises can be done daily, and they help overcome the loss of pelvic floor muscle strength that is typical with aging.
However, Kegel exercises only help women whose urinary incontinence is caused by a slackening in their pelvic floor muscles. In women whose incontinence is because their pelvic floor muscles are always tightened, such as in urge incontinence, Kegel exercises can actually increase their problem.
What are some common medications used to treat urinary incontinence?
These are the medications commonly used to treat incontinence. We break them down here by the type of drug.
Anticholinergics
These medications can calm an overactive bladder and may be helpful for urge incontinence. There are various drugs: oxybutynin (brand name Ditropan XL), tolterodine (Detrol), darifenacin (Enablex), fesoterodine (Toviaz), solifenacin (Vesicare), and trospium (Sanctura).
Mirabegron (Myrbetriq)
This drug is used to treat urge incontinence. It works by relaxing the bladder muscle, which can increase the amount of urine your bladder can hold. It may also increase the amount you are able to urinate at one time, helping to empty your bladder more completely.
Alpha-Blockers
Although we don’t treat male incontinence at Craig Ranch, these medications are used for that. They block bladder neck muscles and muscle fibers in the prostate.
Topical Estrogen
Applying low-dose, topical estrogen in the form of a vaginal cream, ring, or patch may help tone and rejuvenate tissues in the urethra and vaginal areas. Taking hormones orally is not recommended for urinary incontinence, as it can actually exacerbate it.
Is Urinary Incontinence Preventable?
Not all cases of urinary incontinence can be prevented, however, the following recommendations may help in controlling urinary incontinence in some people:
- Drinking fewer fluids
- Emptying the bladder regularly
- Avoiding caffeinated beverages
Kegel exercises may also be effective at strengthening the muscles of the pelvic floor which can help to prevent incontinence.

Is there a relationship between urinary incontinence and diabetes?
Diabetes can cause nerve damage in the bladder, urethra, and pelvic floor muscles. These damaged nerves can send signals to the bladder at the wrong time or not at all, leading to incontinence.
Schedule Your Consultation Today!
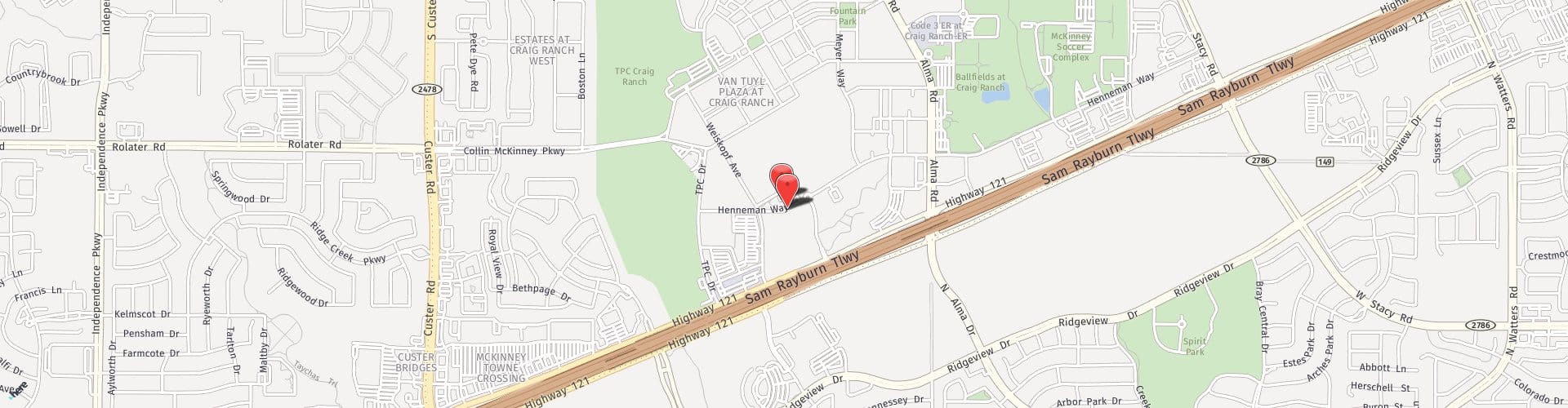
To schedule your consultation, call 214.544.6600. The providers at Craig Ranch OB/GYN are proud to serve patients in McKinney and the surrounding areas of Texas.